Abstract
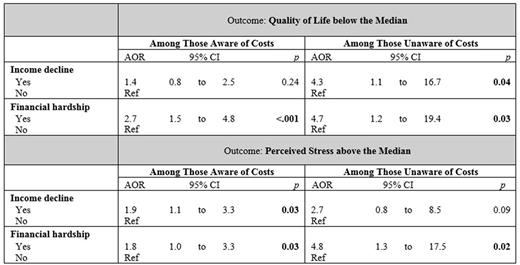
Background: Financial burden during cancer treatment is associated with compromised patient-reported outcomes (PROs). Being aware of impending costs may help preserve affected PROs during treatment, as patients can adjust their financial expectations. We aimed to determine if the relationship between financial burden and PROs differs among those who were aware versus unaware of transplant-related costs before hematopoietic cell transplantation (HCT) for hematologic malignancy. Methods: In 2015, we administered a mailed survey to adult patients at least 150 days after autologous or allogeneic HCT at three centers: Dana-Farber Cancer Institute, Roswell Park Cancer Institute, and Mayo Clinic Arizona. We assessed pre-treatment awareness of transplant-related costs, decreased household income after HCT, and financial hardship (defined as any one or two of the following: reporting being either unsatisfied with present finances, having difficulty meeting monthly bill payments, or not having enough money at the end of the month; given that experiencing all three would represent extreme hardship likely to impact PROs regardless of awareness, we excluded this group). A seven-point scale was provided for perceptions of overall quality of life (QOL, and patient-reported stress was measured with the Perceived Stress Scale (PSS-4). We fit regression models-stratified by awareness-to assess for the association of income decline and financial hardship with QOL below the median and perceived stress above the median (adjusting for transplant type, sex, age, race, marital status, income, distance to transplant center, and time since diagnosis). Results:In the overall survey cohort (n=325; response rate = 65.1%), 21.6% reported being unaware of HCT-related costs, with no differences due to age, race, income, or education as compared to those who were aware. Patients who reported being aware prior to transplant most often reported being informed of costs by a social worker (40.6%) and least often by a physician (23.4%; sources not mutually exclusive). Among aware patients, income decline after HCT was not associated with QOL below the median (AOR 1.4 [0.8, 2.5]; p=0.24); in contrast, among the unaware, income decline increased the odds of reporting worse QOL (AOR 4.3 [1.1, 16.7]; p=0.04). Among the aware, self-reported financial hardship was associated with worse QOL after HCT (AOR 2.7 [1.5, 4.8]; p=<.001), but the odds were even higher among the unaware (AOR 4.7 [1.2, 19.4]; p=0.03). Similar increases were observed among the unaware for the association of decline in income and financial hardship with increased perceived stress. Conclusions: In this large multi-institutional cohort of patients post-HCT, more than one-fifth reported being unaware of transplant-related costs before the procedure. Moreover, this analysis suggests that pre-treatment awareness of transplant-related costs may ameliorate the impact of post-HCT financial burden on patient-reported outcomes.
Khera: Novartis: Consultancy. Zafar: Novartis: Other: Spouse's Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal